TRICHOTILLOMANIA
- Introduction
Trichotillomania is a traumatic, non-scarring alopecia, an obsessive-compulsive disorder or stereotyped motor disorder (OCDs) . The disease is characterized by hair pulling in any position, repeated leading to hair loss but due to the patient’s own actions.
- Epidemiology
- Usually starts in the teenage, adults who has less activity.
- Incidence up to 3.5%.
- Female/male ratio = 9/1.
3 . CLINICAL
– The area of asymmetrical hair loss , polymorphism and unevenness
– T -minded fractures in different lengths, average hair density FREQUENTLY ng, hair pull test is negative.
(Hair pulling test is used to assess the progression of hair loss: grasp about 50-60 hairs jerk from the root to the tip. Positive test when there are 6 hair loss, indicating that the process of hair loss is progressing However, if 3 strands of hair are shed in different areas of the scalp, this test is also considered to be positive)
– The location of hair loss can be on the scalp (usually the top and forehead), eyebrows, eyelashes, pubic hair and often more than one location.
– Often accompanied by some other motor activities such as sucking or biting nails . In some cases, chewing and eating hair lead to bowel obstruction caused by a tufts of hair (trichobezoar).
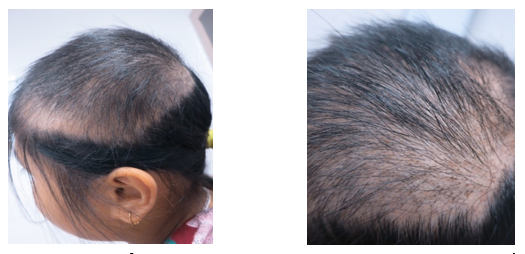
8 year old female patient with the hair loss area cause by trichotillomania.

Images of hair loss with varying degrees of length, position of forehead and top of head
(Source: Internet)
Investigation
– Trichoscopy : 2 quite specific signs in the disease :
+ Broken hair with lots of different lengths
+ Flame hair sign with head fractures fuzzy hair like the shape of the flame
- It is a very specific sign for hair pulling and not seen in other diseases
- It is the result of restoring the rest of a healthy hair after being subjected to strong traction and is less likely to occur in fragile and brittle hair.
+ In addition, you can see signs of black dot, twisted hair, V-shaped …

Different short hairs and flames (red arrows), Bleeding around hair follicles (black arrow) and split hair (red arrow)
5 . DIAGNOSE
– Diagnosis of hair pulling : DSM-IV criteria are:
- Recurrent pulling out of one’s hair resulting in noticeable hair loss.
- An increasing sense of tension immediately before pulling out the hair or when attempting to resist the behavior.
- Pleasure, gratification, or relief when pulling out the hair.
- The disturbance is not better accounted for by another mental disorder and is not due to a general medical condition (e.g., a dermatological condition).
- The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
– Severe diagnosis: based on Massachusetts General Hospital Hairpulling Scale.
6 . DIFFIRENT DIAGNOSTIC
– Alopecia anterior due to other causes .
– Fungal scalp.
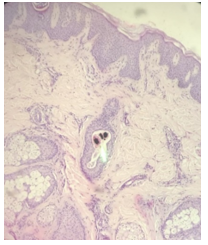
Pigment in hair follicles
7 . TREATMENT
7.1. Specific treatment
– No use of drugs is the first option, including : educating patients, psychotherapy , hypnosis .
– Using drugs : There are currently 3 drugs that prove effective in hair pulling.
+ Olanzapin: antipsychotic drug. In Van’s study, 25 patients with hair loss were randomly divided into 2 groups receiving olanzapine once a day, starting as low as 10mg, then increasing the daily dose depending on clinical response and placebo for 12 weeks. Results 85% (11/13) of patients in the drug group improved compared to 17% of patients in the control group. The average dose of 10.8 ± 5.5 mg / day. Note side effects such as drowsiness, weight gain (about 10% of patients).
+ Fluoxetine : reuptake inhibitor receptors of serotonin (SSRIs), the dose used 60 mg / day , the effect on the individual case.
+ N-acetylcysteine .
7.2. About N-acetylcysteine
– Dosage of 1200 mg / day for the first 2 weeks, then 1200mg / day x 2 times / day for 3-4 months. For adults who have proven effective, children who are effective are uncertain.
– Grant tested 50 patients with adult hair pulling in two randomly divided groups: group 1 received N-acetylcysteine 1200mg twice daily, group 2 took placebo for 12 weeks. Results: 56% of the placebo group had a good and very good effect compared to 16% in the placebo group, after 9 weeks of treatment, there was a difference in effectiveness between the 2 groups, no side effects were noted. However, in Bloch’s study, using the same regimen in 39 children aged 8-17 years saw 25% in the responsive group compared with 21% in the control group, the difference was not statistically significant. In this study, the author concluded that N-acetylcysteine has no effect on hair pulling in children.
REFERENCES
- Pereyra A.D. và Saadabadi A. (2019). Trichotillomania. StatPearls. StatPearls Publishing, Treasure Island (FL).
- Johnson J. và El-Alfy A.T. (2016). Review of available studies of the neurobiology and pharmacotherapeutic management of trichotillomania. Journal of Advanced Research, 7(2), 169–184.
- Grant J.E., Odlaug B.L., và Kim S.W. (2009). N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry, 66(7), 756–763Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: A double-blind, placebo-controlled study. Arch Gen Psychiatry. 2009; 66:756–63.
- Bloch MH, Panza KE, Grant JE, Pittenger C, Leckman JF. N-acetylcysteine in the treatment of pediatric trichotillomania: A randomized, double-blind, placebo-controlled add-on trial. J Am Acad Child Adolesc Psychiatry. 2013;52:231–40.
- Van Ameringen M, Mancini C, Patterson B, Bennett M, Oakman J. A randomized, double-blind, placebo-controlled trial of olanzapine in the treatment of trichotillomania. J Clin Psychiatry. 2010;71:1336–43.
Author: Nguyễn Doãn Tuấn
Publisher: Social Work Department